Situation
The NHS screening services for breast, cervical and bowel cancer are all supported by one digital organisation, responsible for the digital transformation of those services (12 separate services in all). The project situation was challenging:
- There is was no common understanding of patient touchpoints across the thirteen screening patient journeys
- Infrastructure procurement was exacerbating an already complex situation
- The cohort management and screening data storage solutions were “burning platforms”
- Stakeholders were focused on digital and ignoring multichannel or system interactions
- Politics were made more challenging by a complex network of vendors leveraging vested interests
My challenge
My role was to uncover and synthesise the user insights enough to allow my customer to make difficult decisions about what to do next.
The complexity in the patient journey for screening was not so much in the multiple processes, but in the multiple channels through which the patient's needs were addressed (or underserved). My work identified issues with physical location of machines, language used on hospital signage and multiple other touchpoints.
What I did
Understanding the ecosystem constraints
- Unravel the stakeholder spaghetti (NHS/PHE/others)
- Desk research, onboarding with data, review user interviews
- Primary service design research (role-play workshops with SMEs and stakeholders)
- Policy safari, meeting stakeholders across policy, digital and clinical. How the pieces fit together
Understanding the patient experience.
- Learn the multiple patient journeys
- Understand these journey in the context of a wider preventative medicine context considering the impacts of genetics, culture, economics, education etc.
Understanding the journey across all types of screening (cervical, breast, bowel etc.)
- Build a picture of archetypical patients
- Role play these experiences with all stakeholders and SMEs
- Develop an ‘extensible’ journey that will support a plan to build once and reuse across different screening pathways.
The task was to examine the twelve processes and find overlaps and similarities. The objective was to reuse as much data and technology as possible while minimising disruption to patients and support cohort managers in the trust.
Map out the technology
- Understand the architecture of how patient data is captured, stored, and transferred between devices, buildings, networks and vehicles
- Understand the choices made previously which have set up the tech debt and explore options to think differently about the problem
As there is no central datastore for patient data in the NHS, cohort management happens across a wide range of touchpoints. Establishing these points of connection against the stages of the patient journey is a foundational activity in planing a transformation
Sensemaking and evangelism
- Facilitate a series of design thinking workshops with product and programme leadership to create a collective understanding of the situation and document the challenges to the digital screening service so that leadership could tell the story and win further funding.
- Run ideation with a cross disciplinary team of leaders. Establish the blueprint of the ‘extensible service’ with an emphasis on identifying the “lego pieces” that could be re-used between silos and stakeholders.
- Facilitate strategy sessions to map out the end-to-end service with all the lego pieces and collectively prioritise the elements.
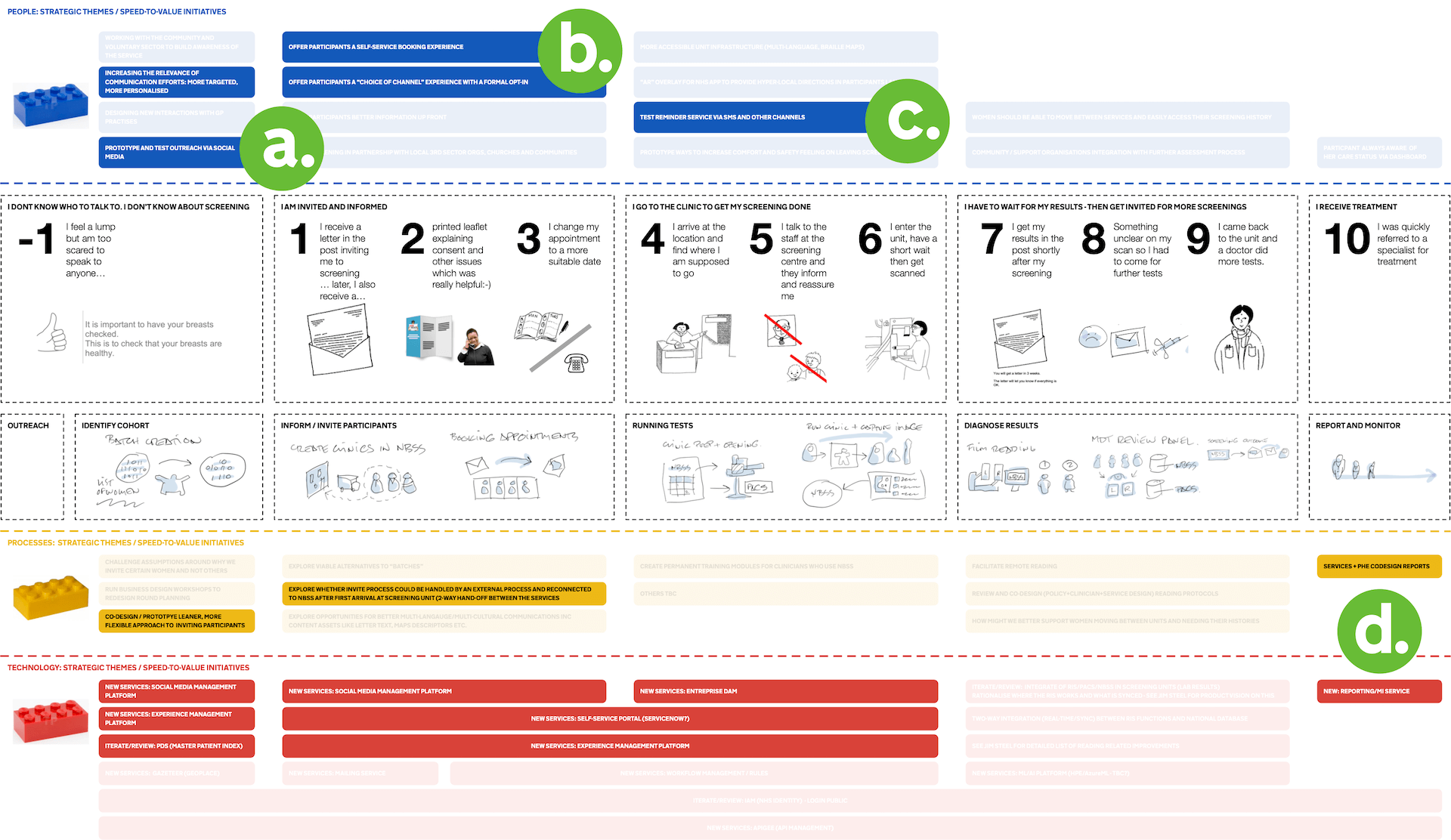
Helping leaders visualise where an intervention can happen both in the lifecycle of the end user and in the front-stage to back-stage dimension. Lego bricks were used to reinforce the idea of modularity and that with the right research, it would be possible to identify the right next steps.
Results
Across the multiple screening patient journeys, four strategic themes or areas of focus emerged and I produced a blueprint document showing the elements to focus on in each of the four themes. Product leadership were then able to build my findings and recommendations into the business case for digital investment.
My stakeholder was successful in their application and the extensible service “mvp” is in production with further screening journeys going live over the coming months.
Can I help you solve a similar problem? dug@goodlookslikethis.com